Lupine Publishers | Advancements in Cardiology Research & Reports
Abstract
Background: In our center, NCTCE, there are 2 intensive care units (general and cardiac), where critically ill patients are
admitted and managed. Anticoagulation is usually indicated in such patients for atrial fibrillation, valve replacement and DVT
prophylaxis.
Objective: To determine the role of a clinical pharmacist in the therapeutic and clinical appraisal of such patients on
anticoagulation.
Materials and Method: Over a 2-year period (June 2015 –May
2017), a study design to determine the role of a clinical
pharmacist in anticoagulant treatment was made in both ICU. This was a
prospective longitudinal study. Here, demography, the
anticoagulation on which interventions were made on, duration of
admission, areas and determinants of a clinical pharmacist’s
interventions were incorporated. Others included, were levels of
intervention, acceptance and rejection of the interventions as well
as the outcome.
Results: During the study period, 168 patients were used. Male (72) and female (96), with a female to male ratio of 1:1.3.
Indications for anticoagulation were DVT prophylaxis (14.88%), valves (83.90%) and AF (1.10%). Among the anticoagulants on
which interventions were made on, warfarin was the highest (53.57%) while heparin was the least (2.90%). Duration of admission
ranged from 2-40 days. Areas of intervention were on effectiveness of therapy (18.70%), drug-drug interactions (16.43%), adverse
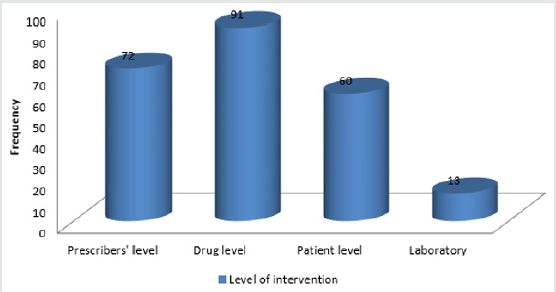
events (32.86%), dosage (11.05%), Kidney function (1.70%), adherence (6.70%) and drug selection (2.27%). Levels of intervention
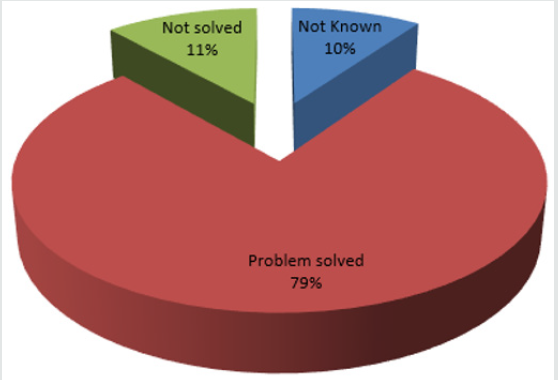
were at prescriber (30.51%), drug (38.56%), patient (25.42%) and laboratory (5.51%). The outcome was that majority of patients
(78.74%) had their problems resolved.
Conclusion: Anticoagulation therapy of patients in ICU requires precise damaging, monitoring and appropriate patient
education so as to ensure that patients benefit maximally. A clinical pharmacist has a vital role to play in the above areas.
Abbreviations: ICU: Intensive Care unit; PhRs: Pharmacist Recommendations; INR: International Normalized Ratio; ACCP:
American Critical Care Physician; ADES: Adverse Events; VTE: Venous Thromboembolism; DTPS: Drug Therapies; DDI/DFI: Drug
Drug/Dug Food Interactions; LMWH: Low Molecular Weight Heparins; CVP: Central Venous Pressure; CHADS: Congestive Heart
failure, Hypertension, Age, Diabetes, Stoke
Introduction
Intensive Care Unit is a unit of the hospital where critically ill
patients are treated by specially trained staff (ICU-Multidisciplinary
team), comprising of doctors, nurse specialists, respiratory
therapists, clinical pharmacists, physiotherapists, dieticians,
theatre technicians, biomedical engineers and social workers. In
our center, there are 2 ICU: -
a) The general ICU for general surgery, orthopedic, neuro-,
obstetrics, thoracic and trauma surgical and medical patients.
b) The cardiac ICU for perioperative open-heart surgery
patients as well as those patients with myocardial infarction
and acute coronary syndromes.
Critical care pharmacy services in the ICU have expanded
from traditional dispensing responsibilities to being recognized as
an essential component of multidisciplinary care for critically ill
patients. Augmented by technology and resource utilization, this
shift in roles has allowed clinical pharmacists to provide valuable
services in the form of assisting physicians and clinicians with
pharmacotherapy decision making, reducing medication errors and
improving medication safety systems to optimize patient outcomes.
Documented improvements in the management of infections,
anticoagulant therapy, sedation, and analgesia for patients receiving
mechanical ventilation and in emergency response help to justify
the need for clinical pharmacy services for critically ill patients [1].
ICU patients have similar general risk factors for
venothrombosis and pulmonary embolism as well as arterial
thromboembolism manifesting as stroke, mesenteric vascular
occlusion and peripheral acute limb ischemia, with other patients
(age, obesity, immobilization, past personal/family history of
venothrombembolism, sepsis, cancer, stroke, respiratory, heart
failure, pregnancy, trauma or recent surgery) [2-4]. In addition, they
have other peculiar risk factors as a result of their illnesses and/
or treatment (vasopressor use, respiratory failure, heart failure,
pharmacologic sedation, mechanical ventilation, central venous
pressure (CVP) catheter and end stage renal failure) [3,5]. CVP
catheter in the femoral, subclavian, internal jugular and superior
vena cava veins have catheter related thrombosis occurrence rate
ranging from 10-69%, 2-10%, 40-56% and 7-17% respectively
[2,5-7]. There is also 4-fold increased risk of pulmonary embolism
from lower limb DVT in ICU patients [8]. Catheter related VTE risks
increases proportionate to the duration of placement and if patient
is not on LMWH anticoagulant [9]. Sepsis induce procoagulant
status and favor catheter related VTE [6,10]. Vasopressor treatment
is not an independent risk factor for VTE [5], however it is still
linked with decreased absorption of subcutaneous heparin due
to the vasoconstriction of peripheral blood vessels [11]. Platelet
transfusion and high platelet levels, a common finding in ICU
patients are risk factors for VTE [12]. Pharmacologic sedation is not
an independent risk factor for VTE, however, when used alongside
mechanical ventilation, it is. Mechanical ventilation by decreasing
venous return and requiring sedation and immobilization is a risk
for VTE, however, critical ill patients requiring long mechanical
ventilation was compared with those who did not and the
relationship between duration of mechanical ventilation and VTE
was not established [2].
The implantation of an artificial heart valves exposes the
patient to an increased risk of valve thrombosis and embolism;
thus life- long oral anticoagulation is imperative [13]. The factors
that lead to increased thromboembolism in such patients are the
number of valves implanted, types of valves implanted (more in
ball and cage variety), atrial fibrillation, left atrial enlargement, left
ventricular dysfunction, clotting disorder and previous embolic
events [14]. Atrial fibrillation is the most common arrhythmia in
patients admitted in intensive care units (ICUs) and is associated
with increased morbidity and mortality [15,16]. The problems of
atrial fibrillation are low cardiac output, heart failure, hypotension
and organ dysfunction as well as thromboembolism. CHADS
algorithm defines the risk factors, which many critically ill patients
have [17]. In addition, patients with rheumatic heart diseases,
prosthetic heart valves, prio thromboembolism and persistent
atrial thrombus detected by TEE as well as AF with complex
atherosclerotic aortic plaque are considered at highest risk of
embolic stroke if not on thromboprophylaxis [18]. In our ICU,
the clinical pharmacist supervises the prescribed anticoagulant,
dispenses them, monitors adverse effects, drug-drug interactions
as well as compliance. These factors among others have a great
role to play in the successful thromboprophylaxis and treatment
of VTE and prevention of anticoagulant induced bleeding including
arterial thromboembolism on account of prosthetic mechanical
heart valves and atrial fibrillation.
Materials and Method
Over a 2-year period (June 2015 –May 2017), a study was designed
to determine the role of a clinical pharmacist in anticoagulant
treatment was made in both general and cardiac ICU of a tertiary
hospital in Nigeria, a developing country. This was a prospective
study. Here, demography, types of anticoagulation intervention
was made on, duration of admission, areas and determinants of
a clinical pharmacist’s interventions were incorporated. Others
included were levels of intervention, acceptance and rejection of
the interventions as well as the outcome. The general ICU admits
critical general, orthopedic, neuro-, thoracic, trauma surgical and
medical patients. The cardiac ICU admits perioperative open-heart
surgical patients including patients with myocardial infarction and
acute coronary syndromes. The data were analyzed using Microsoft
Excel 2010 and presented as frequencies and percentages using
tables and charts.
The study design was approved by the hospital ethical
committee.
Transplantation eligibility is always considered with regard to
risk factors, especially, pulmonary hypertension (Figure 2). Right
heart catheterization must be performed in all potential candidates
for heart transplantation in order to quantify pulmonary vascular
resistance [7]. Right heart failure is a substantial cause of mortality.
Right ventricular failure is likely when post implant pulmonary
artery pressures exceed 50 mmHg. Patients with chronic heart
failure may develop pulmonary hypertension due to elevated left ventricular end diastolic pressure with elevated left atrial
and pulmonary venous pressures. This is a reactive form of
pulmonary hypertension and may fall when the cardiac output is
increased with inotropes or unloaded with nitrate infusions [7].
The transpulmonary gradient is calculated by subtracting the left
atrial filling pressure from the mean pulmonary artery pressure. A
fixed transpulmonary gradient in excess of 14 mmHg is associated
with greatly elevated risk, and thus this cut off is used in the UK [8].
In such patients a destination therapy strategy may be used with
continuous flow LVADS.
Results
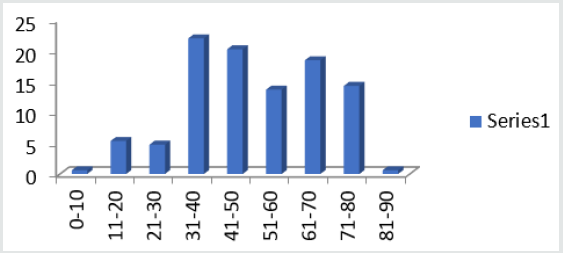
Figure 1 shows the age ranges of patients admitted during the
study period. Highest range is 31-40 years. Least is 81-90 years.
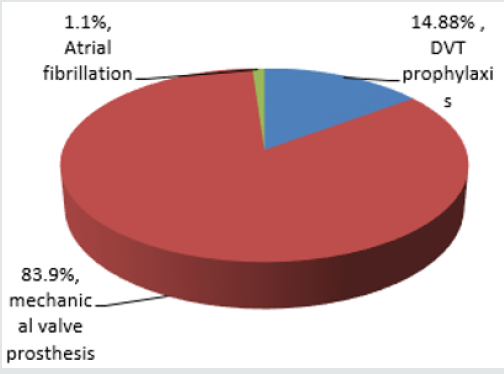
Also Figure 2 shows additional indications for anticoagulation,
with mechanical prosthetic heart valves having the highest
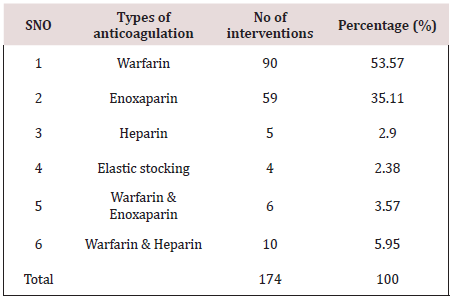
number while atrial fibrillation takes the least. Table 1 shows the
anticoagulants administered and the number of interventions
made on them. The highest number of interventions was made
on warfarin, followed by enoxaparin while the least intervention
was made on nonpharmacologic anticoagulant, elastic stockings.
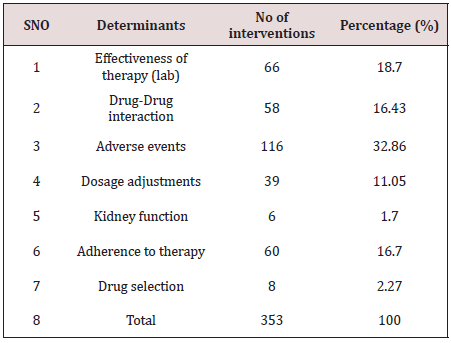
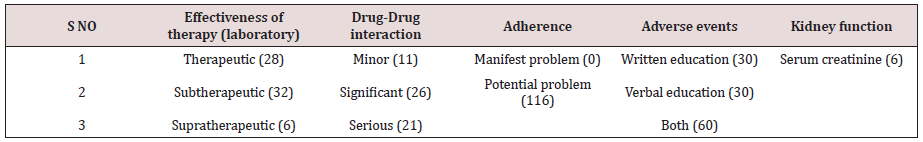
Table 2 of the 353 interventions made, adverse events (32.86%0
was the highest followed by effectiveness of therapy (18.70%),
using laboratory indices of International Normalized Ratio (INR).
The least determinant of intervention was drug-drug interaction
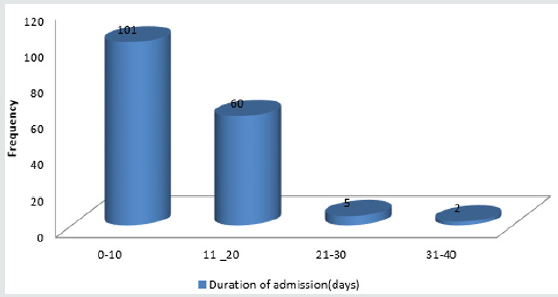
of which (2.27%) interventions were made. Figure 3 depicts
the duration of admission in days. Here the shortest duration of
admission was in most people (66.7%) while the longest admission
in a few patients (1.2%).
Discussion
Intensive care Unit (ICU) is a potential area for drug therapy
problems (DTPs): patients treated are complex patients [19].
The use of thromboprophylaxis or prophylactic anticoagulant
in critically ill patients is pertinent. ACCP recommends
thromboprophylaxis for prevention of VTE in critical care patients
(grade 1a – strong recommendation with high quality of evidence
[20,21]. Omission of thromboprophylaxis within the first 24 hrs of
ICU admission without obvious reasons is associated with a higher
risk of mortality [22]. Demographically, 168 patients admitted in
ICU over 2 years (84-patients/year) had anticoagulation therapy. 96
females and 72 males were involved with a ratio of 1.3:1. The
age ranges were from 0-10 to 81-90 years with highest number
that received anticoagulation being 31-40 years. The bulk of those
with valve prostheses replacement came from this group. Duration
of anticoagulation therapy paralleled relatively the duration of
admission in ICU. In this study, the longest duration was 40 days
while the least was 5 days. Overall, the average length of hospital
stays amounted to 0.24 day/patient. Prospective evaluation of
daily pharmacist-managed inpatient anticoagulation services was
compared with a matched historical control group who received
physician-managed anticoagulation in a 400-bed university
teaching hospital [23]. *26A. Those who received pharmacistmanaged
anticoagulation had significantly shorter hospital length
of stay (6.8 days vs 9.5 days, P 5 .009), fewer supratherapeutic INR
3.5 (27% vs 62%, P , .001),Fewer readmission rates for bleeding or
thrombosis within 1 to 3 months after discharge and no differences
were noted between the groups INR ratio at discharge (2.6 vs 3.3, P
5 .07) as well as number of bleeding complications (6 vs 1, P 5 .11).
Pharmacists have been incorporated into ICU multiprofessional
staff to improve the care provided to patients,
particularly by monitoring the drugs administered and assessing
their efficacy, thus contributing to improving patient safety
[24]. The participation of clinical pharmacists in routine ICU
care mainly includes active involvement in daily rounds, where
they provide relevant information to the medical and nursing
staff, analysis and monitoring of the efficacy of pharmacological
treatments, implementation of medication reconciliation, and
prevention, identification, and reporting of adverse reactions
[25-27]. The actions performed by clinical pharmacists relative
to the monitoring of pharmacological treatment are referred to
as pharmacist interventions or recommendations (PhRs) [24,28].
Such professional interventions presuppose actions targeting
pharmacological treatment to correct or prevent negative clinical
outcomes derived from the use of medications. In the light of the
above, the pharmacist role in the anticoagulant therapy for patients
admitted in our institutional ICU was done. His/her actions in
managing patients in anticoagulation in ICU in terms of monitoring
of the pharmacological therapy of the anticoagulants are referred
as interventions or recommendations. There have been several
reports related to such interventions internationally in patients
admitted in ICU [1,29]. Similar reports are rare in developing
countries like Brazil including Nigeria. A retrospective chart review
conducted at Baylor College in USA, in 2000 [30], showed four main
variances related to warfarin therapy. They were inappropriate
administration of warfarin loading dose, use of vitamin K when not
recommended by American College of Chest Physicians guidelines,
inconsistent overlapping of heparin with warfarin and inconsistent
provision of patient education [30]. In this study, the determinants
of the interventions ranged from effectiveness of therapy to drug
selection, see Table 2. With this subgroup of effectiveness of therapy,
international Normalized Ratio was used to monitor dosages
which enabled the pharmacist to classify them as sub therapeutic,
therapeutic and supratherapeutic.
In this same scenario, drug-drug or drug-food interactions
were monitored and classified as minor, significant or serious,
see Table 3. When the effectiveness of therapy was supra or sub
therapeutic, and when the DDI/DFIs were significant or serious,
pharmacist intervened or made recommendations. The same
scenario applied to adverse reactions, adherence to therapy as well
as kidney function. These recommendations were made at multiple
levels ranging from physicians/prescribers’ level to laboratory
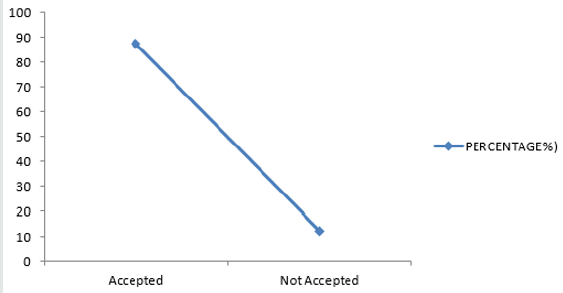
level. In view of the fact this pharmacist’s interventions or
recommendations are novel in our institution and indeed in Nigeria, many
interventions were accepted while some were rejected, see
Figure 4. The outcome of such interventions is shown in Figures 5 &
6, indicating excellence when such recommendations are accepted.
In a prospective, interventional study in a multidisciplinary ICU
of a rural district hospital in Bathalapalli, Andhra Pradesh, India
by Pichala et al. 72 patients were screened for DTPs, 947 drug
doses prescribed, 148 prescriptions, 6.39 drugs per prescription
and 13.15 drugs per patients of 243 DTPs identified, 1.67 DTPs
present were prescriptions, drug interactions 78%, inappropriate
indication 7.4%, ADRs and therapeutic duplications 2%. 47% of
the interventions were accepted. This was significantly lower when
compared with our study. ICU SUCCESS DEDICATED PHARMACIST
study done by Leape et al., concluded that: participation of
the pharmacist on medical round can be a powerful means
of reducing the risks of ADEs, in the ICU 99% of pharmacist
recommendations to medical staff were well accepted, an existing
pharmacist intervention required no additional resources; instead
it represented a different use of existing pharmacists’ time.
Conclusion
Anticoagulation treatment of patients in ICU requires precise
dosing, a defined anticoagulant management programme, approved
protocols, proper monitoring by clinical pharmacist (base line and
follow-up INRs), education of patients and families about: dietary
restrictions, monitoring follow up, drug interactions for outpatient
and inpatient components. All these will result in improvement in
the INR results, significant clinical outcomes and overall quality of
care.
For
more Lupine Publishers Open
Access Journals Please visit our website
https://www.lupinepublishers.com/
For more Journal of Cardiology & Clinical Research Please Click Here:
For more Journal of Cardiology & Clinical Research Please Click Here:
To Know more Open Access Publishers Click on Lupine Publisher
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online