Introduction
Read More about Lupine Publishers Google Scholar Articles:
Introduction
Read More about Lupine Publishers Google Scholar Articles:
Happy thanksgiving!
"May
all the good things of life be yours, not only on this day, but throughout the
coming year."
"Wishing you a harvest of blessings, good health and good times." "May
you enjoy a bountiful Thanksgiving, a joyous holiday season and healthful,
Happy New Year." From Lupine publishers Group💌
Hypertension is a global public health issue that affects approximately 1 billion people worldwide in both developed and developing countries. It is also considered as an ‘Iceberg’ disease’ because unknown morbidity far exceeds the known morbidity. High blood pressure (BP) is ranked as the third most important risk factor for at attributable burden of disease in South Asia. With an aim to determine the profile of the hypertensive patients a retrospective cross-sectional study design was used to analyze the medical record of 1311 patients admitted with the primary diagnosis of hypertension at BPKIHS January 2005 to May 2016. The study revealed that majority (82.4%) of the patients was above 40 years of age with the mean age of 57.14 ±17.5. More than half (53.5%) of the patients were male. Almost half (49.4%) of the patients were from Sun sari district. More than 90% of the patients were admitted in medical ward. Majority (90.7%) of the patients were improved at the time of discharge.
Read More About This Article Click on Below Link:
https://lupinepublishers.com/cardiology-journal/fulltext/profile-of-patients-admitted-with-hypertension-at-a-tertiary-level-hospital-of-eastern-nepal.ID.000102.php
Read More about Lupine Publishers Google Scholar Articles:
https://scholar.google.com/citations?view_op=view_citation&hl=en&user=EuBF0zMAAAAJ&citation_for_view=EuBF0zMAAAAJ:UY3hNwcQ290C
Lupine Publishers | Advancements in Cardiology Research & Reports
Fast Brain MRI Protocol: Use of limited-sequence Brain MRI to confirm the diagnosis of stroke and identify ‘Stroke Mimics’ after negative initial neuroimaging following stroke thrombolysis.
Keywords: Stroke; Thrombolysis; Fast MRI (Magnetic resonance Imaging with limited sequence); CT-head (computerised Tomography of the head)
Various studies have shown that a significant proportion of patients presenting as acute ischaemic stroke and thereby receiving stroke thrombolysis may have ‘Stroke Mimics’. Due to the time constrain in differentiating the true stroke from stroke mimics and limited availability of the timely MRI head these patients are not identified at stroke thrombolysis. However, diagnostic clarity is necessary thereafter for the appropriate management of such patients. A limited sequence ‘Fast Brain MRI protocol’ was introduced in our stroke unit to identify such ‘Stroke Mimics’ after thrombolysis. This 5-minute fast Brain MRI protocol included axial FLAIR and DWI sequence.
We evaluated all acute ischaemic stroke patients receiving thrombolysis in a DGH over 12 months. All thrombolysis patients received a routine CT Head 24 hours after receiving thrombolysis. Those patients with negative neuroimaging for an infarction at 24 hour received MRI Brain. A limited-sequence ‘Fast Brain MRI protocol’ was introduced in our stroke unit, this 5-minute fast Brain MRI protocol included axial FLAIR and DWI sequence[1].
Out of total 1200 patents referred with a possible diagnosis of stroke or stroke-like event over the 12 months between August 2017 to July 2018, 223 patients were within the thrombolysis window. 53 of them received stroke thrombolysis (thrombolysis rate 24%)[2]. f 14 out of these 53 patients (26%) were neuroimaging negative at 24hour CT and hence ended up having Fast MRI of their head. Out of this 14 thrombolysed but initial neuroimaging-negative patients 6 patients (11% of total thrombolysed cases) were noted to have DWI-negative MRI Brain scan and hence identified as ‘Stroke Mimic’ who has received thrombolysis. Out of 14 thrombolysed but initial neuroimaging-negative cases 64% (9 out of 14) were confirmed to have a stroke after MRI scan and 36% (5 out of 14) were negative for any recent infarction (Table 1 & 2).
In our study, we noticed that the majority of patient with suspected acute ischaemic stroke and thereby receiving stroke thrombolysis were confirmed to have a cerebral infarction. Only 11% of thrombolysed stroke was confirmed as ‘Stroke mimic’. We concluded that thorough initial assessment and full NIHSS scoring had taken place in all these cases before thrombolysis. Unless a ‘Fast Brain MRI’ scan protocol is readily available without any delay prior to stroke thrombolysis it would not be possible to completely exclude the stroke, mimics receiving thrombolysis; as there is always anxiety that we might deny the thrombolysis to the genuine patients otherwise.
For more Lupine Publishers Click on Below link
Lupine Publishers | Advancements in Cardiology Research & Reports
Keywords: LVAD implantation; non-cardiac surgery; atypical lung resection
Indications to continuous flow left ventricular assist devices (CF-LVAD) have significantly broadened over the last decade considering even old patients with cardiac and extra-cardiac comorbidities [1]. Concomitant cardiac procedures to LVAD implantation are well described since nowadays up to 35% of implantations require concomitant cardiac surgery including valvular surgery, coronary artery bypass grafting, ventricular arrhythmias ablation, and atrial septal defects repair [1]. But the impact of these concomitant procedures is not well studied and guidelines are lacking. In particular for non-cardiac surgery experiences are limited to case series and the decision-making is driven on a single patient basis. To our knowledge, concomitant LVAD implantation and lung surgery has not been described before. We report the case of a patient who underwent a second generation CF-LVAD implantation followed by an atypical right lower lobe resection.
A 56-year-old man mildly obese and previous heavy smoker, presented with post-ischemic dilated cardiomyopathy and severely decompensated heart failure (orthopnea, dyspnea, fluid retention, and weight gain) with left ventricular ejection fraction (EF) of 17%. He also showed non-reversible post-capillary pulmonary hypertension and right ventricular (RV) dysfunction: Tricuspid Annular Plane Systolic Excursion (TAPSE) of 10 mm, RV Fractional Area Change (RVFAC) of 20%, Right Ventricular Stroke Work Indexed (RVSWI) of 400 mmHg/ml/m2 and a central venous pressure to wedge pressure ratio of 0.8. Few days after admission the patient developed hemoptysis. A 15-mm enhanced contrast lung nodule in the latero-basal segment of the right lower lobe (RLL) with a maximum standardized uptake value of 8, was demonstrated at the Positive Emission Tomography Scan (Figure 1A). The CT-scan showed a nodule suspicious for neuroendocrine tumor because of early contrast enhancement and a regular profile. Due to its peripheral position the nodule could not be reached with a transbronchial biopsy and a percutaneous computer tomography guided biopsy was considered to be too high risk. The pulmonary function tests were normal despite the presence of centrilobular and paraseptal emphysema.
Figure 1: (A)Computer Tomography and Positron Emission Tomography scan showing RLL enhanced contrast nodule; (B) manual palpation of lung nodule with deflated lung; (C) wedge resection of the RLL; (D) histology of the lung lesion showing a complex artero-venous malformation.
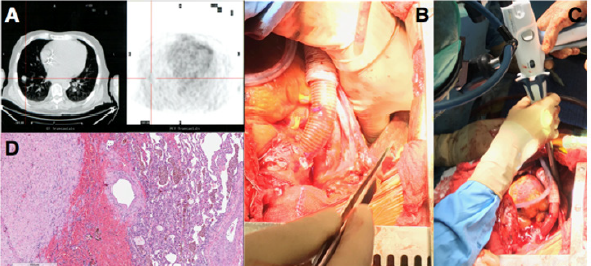
He showed a positive clinical response to an aggressive diuretic therapy with significant reduction in weight and fluid retention, and improvement in right ventricular function (TAPSE 17 mm, RVFAC 33%, RVSWI 600 mmHg/mL/m2, central venous pressure to wedge pressure ratio of 0.4) which allowed to list the patient for an LVAD implantation. Considering right ventricular improvement, favorable position of the lung nodule and the complex coagulation management of a staged approach a combined procedure was preferred. A 24 hours infusion of levosimendan was completed in the immediate preoperative period. In consideration of the presence of the pulmonary lesion, we decided for a destination therapy configuration of the Jarvik 2000 (Jarvik Heart, Inc, New York, NY, USA) with an intraoperative retroauricolar implantation of the pedestal. After fixation of the pedestal, the pericardial space was approached via a median longitudinal sternotomy. Once the driveline was tunneled, LVAD implantation inside the left ventricle apex was performed on cardiopulmonary bypass (CPB) and beating heart, the outflow conduit was sutured to the ascending aorta. The progression from CPB to LVAD level 2 support was facilitated by continuous infusion of epinephrine (0.04 mcg/kg/min), norepinephrine (0.05 mcg/kg/min) and 20 ppm of inhaled nitric oxide to facilitate RV function.
When surgical and medical hemostasis were carefully achieved, one lung ventilation with 5 mL/Kg tidal volumes was initiated and a positive end expiratory pressure of 8 cmH2O, inhaled nitric oxide was increased to 30 ppm. Even if the PaO2/FiO2 ratio was 100 mmHg and the PaCO2 was 47 mmHg, the TEE showed normal RV function with a pulmonary artery systolic pressure of 40 mmHg. RLL exposure was achieved through the mediastinal pleura via the median sternotomic access. Manual palpation with inflated and noninflated lung allowed nodule identification and wedge resection of the RLL with an Echelon Flex 60 Endopatch (Ethicon Endo Surgery Inc., Cincinnati, OH) (Figure 1 B,C). Pathological examination demonstrated a complex artero-venous malformation (Figure 1D). The patient had an uneventful postoperative course with weaning from mechanical ventilation and inotropic support within the first 36 postoperative hours. He was discharged from the postoperative intensive care unit on day 6 and on day 17 to a rehabilitation center. Since the lung lesion was benign the patient was eligible to enter the heart transplantation list discharged and strictly monitored with a telemedicine program previously described [2].
The population of patients eligible for LVAD implantation has broadened over the last years and thanks to the reported improvements in mid-term outcomes and quality of life, the number of patients scheduled for a concomitant non-cardiac surgery intervention has progressively increased [3]. Planning a combined procedure in these fragile patients requires a thorough multidisciplinary approach, a strict preoperative medical optimization and the design of an effective and safe surgical procedure. Few cases of thoracic surgery in patients with CFLVAD have been published [4,5]. In this case, surgical plan was carefully defined in consideration of the major perioperative risks. Great attention was paid to RV function and preservation since hemodynamic changes following LVAD implantation are difficult to predict and have a huge impact on results [6,7]. Since no data have been published on the relationship between the amount of lung parenchyma excised and the variation of pulmonary resistances and thus of right ventricular afterload, we have chosen a step-bystep approach. An atypical lung resection was first performed. A RLL lobectomy would be a second surgical step only in case of demonstrated malignancy, minimizing in this way right ventricular impact and allowing a gradual adaptation of the RV to increased pulmonary resistances. During the procedure RV function was evaluated through surgical visual inspection, TEE and right heart catheterization allowing for immediate pump speed variations or pharmacological support titration.
The delicate interaction between RV, mechanical ventilation and hypoxia has been largely described in the population of patients suffering from acute respiratory distress syndrome and also during the intraoperative management of one lung ventilation for thoracic surgery, but it has never been studied in the context of LVAD support [8]. Indeed, RV disfunction after LVAD implantation is a life threating complication that can occur in 20 to 50% of patients [9] especially in the presence of high pulmonary vascular resistances. The RV showed a positive response to the increased venous return, to the geometrical adaptation of the interventricular septum and the augmented pulmonary vascular resistances. The favorable anatomical position of the lung nodule allowed to employ the median sternotomy for both LVAD implantation and lung resection. Concomitant procedure reduced the perioperative bleeding and infective risks. This case underlines the crucial role of a multidisciplinary approach, a preoperative medical optimization, a step-by-step surgical plan and a multimodal right ventricular evaluation.
For more Lupine Publishers Click on Below link
Lupine Publishers | Advancements in Cardiology Research & Reports
Cardiovascular disease (CVD) encompasses a broad range of conditions. Coronary Artery Disease (CAD), commonly referred to as Ischemic Heart Disease (IHD), is the leading cause of death, morbidity, and mortality in the United State and women continue to have poorer outcomes than men. The causes of these discrepancies have yet to be fully elucidated. In this review, we reported gender-based studies of diagnosis, treatment, and outcome of CVD in the last 20 years.
Keywords: Cardiovascular disease; gender-based discrepancies; diagnosis; treatment
Cardiovascular disease (CVD) is the major cause of death in the United State and other countries [1]. Age, ethnic, racial, and gender differences within CVD diagnosis and treatment have been well reported in several studies. Because men and women have different characteristics and predictive factors, decision-making based on the currently standardized frameworks and recommendations for clinical diagnosis and treatment tend to lead to poorer outcomes in women compared to men. In this paper, we present a short review of a few related works in gender-based CVD-related studies over the past 20 years.
In 1999, Kameneva MV et al. [2] reported that CVD mortality in men and menstrual women, particularly myocardial infarction (MI), is significantly higher than pre-menopausal women, which may be associated to the difference in age of red blood cells and the consequent differences in the structural features of menstrual and postmenopausal women. According to their results, men have hematocrite, blood viscosity, RBC aggregation, and RBC rigidity higher than pre-menopausal women. Jeanine E Roeters van Lennep et al. [3], concluded that diabetes, high density lipoproteins, and triglyceride levels were found to have a greater effect on women’s risk of coronary heart disease than men. They also found out that women and men show different responses to risk factors or to treatment in case of optimal treatment and prevention. In a research done by Edgar Argulian et al. [4], they suggested that women were more likely to experience coronary artery injury and bleeding problems than men, despite similar high angiographic and procedural success rates of PCI for both sexes. According to Regithz Zagrosek et al. [5], the increased prevalence of MetS in women over 40 years was 76% compared to 5 percent in men at the same age. In the cardiovascular risk associated with diabetes mellitus and hyperglycemia, the same gender difference was also observed.
In a study conducted by Kwok Leung Ong et al. [6], they suggested that sex hormones could be responsible for gender differences in coordination with blood pressure. Even though there was higher diastolic blood pressure in men, higher systolic pressure was reported in women which is a greater risk factor for CVD. They found that women had more prevalence of cardiovascular risk factors such as central obesity, high total cholesterol, and low HDL than men. Giusepp Mercuro et al. [7] reported significantly higher mortality rates among women with diabetes compared to men of the same age and women were less likely to ask for medical help. According to their report, women of older age have the nonischemic disease in patients with heart failure and have more severe symptoms of heart failure. By increasing the risk of a first acute myocardial infarction (AMI), smoking is more dangerous in younger women (< 50 years) than in men according to Maas AH et al. [8]. They also presented that Smoking also induces a downregulation of estrogen-dependent vasodilatation of the endothelial wall in young premenopausal women that can contribute to more problems in CHD patients. G Penno et al. [9] found that while CVD was more common in men, women had a greater risk profile for CVD and worse outcomes for therapy. They concluded that women were less likely to receive pharmacological therapy for hypertension hyperglycemia and dyslipidemia than men. In an exclusive analysis of a national cohort of CVD, Salim S. Virani et al. [10] found women were less likely to take statins and high-intensity statins than men did. Also, significant facility-level variation in both statin and highintensity statins used in female patients was observed.
Ramzi Y Khamis et al. [11] discovered that CVD diagnosis has been shown to be poorer since women with chest pain were less likely to perform ECG exercise and less probable to have coronary angiography. They stated that Females tend to experience CVD later in life and appear to be treated with less certainty than their male counterparts even when diagnosed. It has also been shown that women respond to antiplatelet agents differently from men, so residual platelet activity appears to be higher in them. According to Min Zhao et al. [12] report, women are worse at managing risk factors in CHD prevention. Results showed better regulation of blood pressure in women, but they had a poorer profile in glucose and lipid therapy target levels. Women tended to undergo less rigorous lipid-reduction therapy than men. Upon cardiovascular events, they were also less likely to take aspirin, ACE inhibitors, or statins. Niti R. Aggarwal et al. [13] suggested that considering advances in IHD mortality, it is still the leading cause of death among women. Compared to men, women are much less probable to be detected and involved in cardiac rehabilitation. Also, there are several non-traditional cardiac complications in women, including early menopause and menarche, gestational diabetes mellitus, and hypertension. In 2019, Amy Johnson et al. proved that women were more likely to die within one year of cardiac surgery and long-term follow-up than men. They also found that despite the fact that a higher mortality rate among women was correlated with remote MI, recent MI and previous PCI, there was a lower risk of death among men who had previous PCI [1].
The review of related works shows significant works and finding around risk factors and outcomes in CVD for men and women. But the causes of these discrepancies have yet to be fully addressed and require further research in this field of study to overcome poorer outcomes in women. Further detailed analysis is needed in order to design interventions and structures to minimize bias. The complication of pregnancy and other women-specific situations make it difficult to diagnose female patients with CVD in a timely manner.
For more Lupine Publishers Click on Below link
Lupine Publishers | Advancements in Cardiology Research & Reports
It is important to predict Kawasaki Disease (KD) patients who will be resistant to Intravenous Immunoglobulin (IVIG) before starting the initial treatment, as these patients may have severe inflammation and vasculitis, which will likely lead to the development of Coronary Artery Lesions (CALs). An intensive initial treatment combined with IVIG and additional anti-inflammatory drugs is reported to reduce the occurrence of IVIG resistance and CALs. Although risk scoring systems using usual laboratory data to predict IVIG-resistant patients have mainly been developed in Japan, these systems did not accurately predict non-responders to IVIG among patients in the other countries. In this review, we provide a comprehensive overview of the main risk scoring systems and evaluate the relevant literature.
Kawasaki Disease (KD) is an acute systemic vasculitis that mainly occurs in infants and young children [1]. Although intravenous Immunoglobulin (IVIG) is an effective treatment for KD [2], approximately 10-20% of KD patients are resistant to IVIG therapy [2,3]. IVIG-resistant patients with KD have a higher risk of developing coronary artery lesions (CALs) than responders to IVIG therapy [4,5]. It is important to predict IVIG-resistant KD patients before starting the initial treatment, because intensive initial combination therapy with IVIG and other anti-inflammatory drugs, such as Ulinastatin [6], steroid [7,8] and infliximab [9], may reduce the occurrence of IVIG resistance and/or CALs. There are several risk scoring systems for predicting IVIG resistance in KD patients; the Kobayashi [10], Egami [11] and Sano [12] risk scores have been commonly used in Japan. Recently, we reported a new risk scoring system using two blood cell subtype ratios, the neutrophil-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) [13]. Furthermore, several researchers have reported other risk scoring systems in such countries as the U.S. [14], Taiwan [15] and China [16-18]. The aim of this review is to compare the predictive validity among these risk scoring systems and assess their problems and limitations.
The main risk scoring systems for predicting the IVIG resistance in KD, which have been reported to date, are summarized in Table 1. The parameters of the Egami score [11] consist of alanine aminotransferase (ALT) ≥80 IU/L (2 points), age ≤6 months (1 point), days of illness ≤4 days (1 point), C-reactive protein (CRP) ≥8 mg/dl (1 point) and platelet count ≤300×103/mm3 (1 point). In the high-risk group (score ≥3), the sensitivity and specificity in the prediction of IVIG resistance were 78% and 76%, respectively. The parameters of the Sano score [12] consist of Aspartate Amino Transferase (AST) ≥200 IU/L (1 point), CRP ≥7 mg/dl (1 point) and total bilirubin ≥0.9 mg/dl (1 point). In the high-risk group (score ≥2), the sensitivity and specificity in the prediction of IVIG resistance were 77% and 86%, respectively. The parameters of the Kobayashi score [10] consist of sodium ≤133 mmol/L (2 points), days of illness at initial treatment ≤4 days (2 points), AST ≥100 IU/L (2 points), % of neutrophils ≥80 (2 points), CRP ≥10 mg/dl (1 point), age ≤12 months (1 point) and platelet count ≤300×103/ mm3 (1 point). In the high-risk group (score ≥4), the sensitivity and specificity in the prediction of IVIG resistance were 86% and 68%, respectively. Recently, Kawamura et al. reported that the combination of NLR ≥3.83 and PLR ≥150 is a useful predictor of IVIG resistance in KD [13], and the sensitivity and specificity of NLR ≥3.83 and PLR ≥150 in the prediction of IVIG resistance were 71% and 69%, respectively. These simple ratios are convenient and costeffective in comparison to other scoring systems.
Table 1: Risk scoring systems predicting IVIG resistance in KD patients.

ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C-reactive protein; GGT, γ-glutamyl transferase; NLR, neutrophil- lymphocyte ratio; PLR, platelet to lymphocyte ratio; PLT, platelet; zHgb, age-adjusted hemoglobin concentration.
In the US, the San Diego score [14] was proposed. The parameters consist of % of bands ≥20 (2 point), illness days≤4 (1 point), γ-glutamyl transferase (GGT) ≥60 IU/L and age-adjusted hemoglobin concentration (zHgb) ≤-2. In the high-risk group (score ≥2), the sensitivity and specificity in the prediction of IVIG resistance were 73% and 62%, respectively. In Taiwan, the Formosa score [15] was reported. The parameters consists of % of neutrophils ≥60 (2 points), albumin <3.5 g/dl (1 point) and positive lymphadenopathy (1 point). In the high-risk group (score ≥3), the sensitivity and specificity in the prediction of IVIG resistance were 86% and 81%, respectively. In China, Fu et al. reported a scoring system. The parameters consist of % of neutrophils ≥80 (2 points), illness days ≤4 (1 point), CRP ≥8 mg/dl (2 pint), polymorphous exanthema (1 point) and change around the anus (1 point) [16]. In the high-risk group (score ≥4), the sensitivity and specificity in the prediction of IVIG resistance were 54% and 71%, respectively. Tang et al. reported another scoring system. The parameters consist of age <6 months (2 points), albumin 3.5 < g/dl (2 points), edema of extremities (1 point), rash (1 point) and % of neutrophils ≥80 (1 point) [17]. In the high-risk group (score ≥3), the sensitivity and specificity in the prediction of IVIG resistance were 71% and 76%, respectively. Recently, Hua et al. reported a new scoring system. The parameters consist of fever duration ≥7 days (2 points), delayed diagnosis (1 point), GGP ≥25 mg/dl (1 point), sodium < 135 mmol/L (1 point), NLR ≥2.8 (1 point) and platelet count ≤350×103/mm3 (1 point) [18]. In the high-risk group (score ≥4), the sensitivity and specificity in the prediction of IVIG resistance were 61% and 67%, respectively. As described above, each of risk scoring systems are determined based on different clinical data and symptoms, although some factors are duplicated among these scoring systems.
There are differences in the definition of IVIG resistance in each study. Egami defined IVIG resistance as persistent fever (≥37.5℃) and a fall in CRP by <50% within 48 hours after IVIG therapy [11]. Sano defined IVIG resistance as persistent fever (≥37.5℃ over 24 hours) after finishing IVIG therapy [12]. Kobayashi and Kawamura defined IVIG resistance as persistent fever lasting >24 hours after the completion of the initial treatment or in the presence of recrudescent fever associated with KD symptoms after an afebrile period [10,13]. The San Diego score defined IVIG resistance as persistent fever (≥38.0℃ rectally or orally) for at least 48 hours but no longer than 7 days after IVIG therapy [14]. The Formosa score defined IVIG resistance as persistent fever or development of recrudescent fever associated with KD symptoms after afebrile period [15]. Fu and Hua defined IVIG resistance as persistent or recrudescent fever at any time 48 hours to 2 weeks after IVIG therapy and at least 1 of the standard diagnostic criteria [16,18]. Tang defined IVIG resistance as recrudescent or persistent fever ≥36 hours after the end of IVIG infusion [17]. Thus, because the definition of IVIG resistance has not been standardized, international consensus will be needed in the near future. In the 2017 Kawasaki disease guidelines from the American Heart Association, the definition of IVIG resistance was recrudescent or persistent fever at least 36 hours after the end of IVIG infusion [19].
Several authors have assessed the sensitivity and specificity of risk scoring systems when they were applied to KD patients in the other countries (Table 2). The Kobayashi risk score (≥4), Egami risk score (≥3) and Sano risk score (≥2) have good specificity (87%, 85% and 85%, respectively) but low sensitivity (33%, 42% and 40%, respectively) for predicting IVIG resistance in KD patients in North America [20]. Similarly, the Kobayashi risk score (≥4), Egami risk score (≥3) and Sano risk score (≥2) have good specificity (87%, 87% and 92%, respectively) but low sensitivity (31%, 34% and 28%, respectively) for predicting IVIG resistance in KD patients in Korea [21]. In KD patients in China, Song et al. reported that the Kobayashi risk score (≥4) and Egami risk score (≥3) have good specificity (85% and 84%, respectively) but low sensitivity (16% and 14%, respectively), the San Diego risk score (≥2) has high sensitivity (95%) but very low sensitivity (3%), and the Formosa score (≥3) has relatively low specificity (47%) and sensitivity (43%) for predicting IVIG resistance [22]. Qian et al. reported that the sensitivity of Kobayashi risk score (≥4), Egami risk score (≥3), Sano risk score (≥2), Kawamura risk score (≥2) and Formosa score (≥3) were 72%, 44%, 20%, 48% and 68%, respectively, and that the specificity of these scores were 62%, 82%, 91%, 66% and 48%, respectively [23]. In the United Kingdom, the Kobayashi risk score (≥4) had relatively low sensitivity (58%) and low specificity (35%) [24]. In the Kobayashi score, a cut-off risk score of 5 points was also reported to be effective for predicting IVIG resistance in Japanese patients with KD [7,25]. The Kobayashi risk score (≥5) is reported to predict IVIG resistance in Iranian patients with KD, with 50% sensitivity and 94% specificity [26].
Table 2: Sensitivity and Specificity of risk scoring systems when applied to different ethnic group.
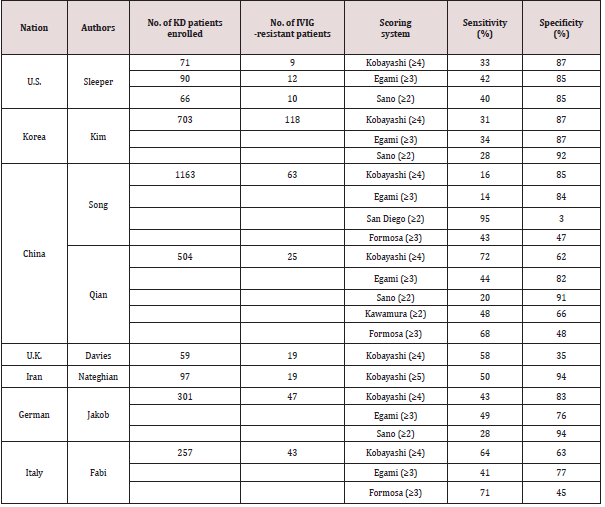
Recently, Jakob et al. reported that the Kobayashi risk score (≥4), Egami risk score (≥3) and Sano risk score (≥2) have low sensitivity (43%, 49% and 28%, respectively), although they have relatively high specificity (83%, 76% and 94%, respectively), in German patients with KD [27]. More recently, Fabi et el. reported that the Kobayashi risk score (≥4), Egami risk score (≥3) and Formosa score (≥3) are ineffective for predicting IVIG resistance (sensitivity: 64%, 41% and 71%, respectively; specificity: 63%, 77% and 45%, respectively) in Italian children with KD [28]. Besides, the ability of NRL and PLR to predict IVIG resistance in KD was evaluated in China: the cut-off values of NLR ≥4.36 and PLR ≥162 were useful for predicting IVIG-resistance in KD [29], and NLR ≥2.51 was useful in KD patients younger than 1 year of age [30]. Although there is a slight difference in the cut-off values of Japan [13] and China [29], the effectiveness of the NLR and PLR in predicting IVIG resistance has been proven in both countries.
Many of the Japanese scoring systems (Egami, Sano and Kobayashi scores) had relatively good specificity but low sensitivity when they were applied to non-Japanese KD patients. These results indicate that the use of Japanese risk scores in other countries can exclude most patients who do not require additional therapy (lowrisk patients) but cannot accurately extract patients who require additional therapies (high-risk patients). For this reason, these Japanese risk scores have not been widely used outside Japan. These regional differences could be due to genetic differences or other environmental factors [31]. It is reported that the functional polymorphism and methylation of the immunoglobulin gamma Fc region receptor II-a (FCGR2A) gene might be associated with IVIG resistance in KD patients [32,33]. As there is a difference in the incidence of KD among countries, the disease severity and the effectiveness of IVIG therapy might also be different. It seems difficult to establish a universal risk scoring system for IVIG resistance in KD due to racial differences. Thus, it might be better to aim to establish discrete risk scoring systems for each country. It would be preferable if the risk score is simple and convenient. The determination of cut-off values for the NLR and PLR in each country may warrant investigation because these ratios are easily calculated. In summary, the prediction of failure to respond to IVIG therapy is important for identifying KD patients who may need additional anti-inflammatory treatments, because intensive therapy can be reduce the incidence of IVIG resistance and CAL formation. Although several risk scoring systems of IVIG resistance have been proposed, many of these failed to effectively predict IVIG resistance in other countries. Further studies will be needed to obtain consensus on a risk scoring system for predicting IVIG resistance in KD.
For more Lupine Publishers Click on Below link
Introduction 53 years old female patient, who presented oppressive precordial pain, radiating to the neck and jaw, for which she went to...